Effects of Sheetali and Sheetkari Pranayamas on Blood Pressure and Autonomic Function in Hypertensive Patients
Prashanth Shetty, BNYS , MSc, PhD ; Kiran Kumar Reddy B, BNYS, MD ; D R Lakshmeesha, BNYS, MD; Shiva Prasad Shetty, BNYS, MSc ; Selva Kumar G, BNYS ; Ryan Bradley, ND, MPH
Abstract
Context: Hypertension (HTN) is a chronic medical condition affecting nearly 1 billion people worldwide. Yoga, typically thought of as a series of physical postures, also includes breath practices and meditation. It has the potential to reduce of blood pressure (BP) through a combination of stress reduction and modification of the physiology of the autonomic nervous system. Pranayama is the art of prolongation and control of breath and helps bring conscious awareness to breathing patterns.
Objectives: The study aimed to measure the effects of Sheetali and Sheetkari pranayamas on BP, the autonomic nervous system, and respiratory functions among hypertensive participants.
Design: The study design was a randomized controlled trial.
Setting: The study was carried out at a clinical research center at Sri Dharmasthala Manjunatheshwara Yoga and Nature Cure Hospital (Belthangady, India).
Participants: The participants were 60 hypertensive individuals, aged from 25 to 65 y, who were recruited from the general population located in and around Ujire, Belthangady, Karnataka, India.
Intervention: Participants were randomly assigned either to an intervention group (n = 30) or wait-list control groups (n = 30). The intervention included 2 types of pranayama breath practices (ie, Sheetali and Sheetkari) each practiced for 10 min/d.
Outcome Measures: BP and autonomic and respiratory functions were measured at baseline and postintervention.
Results: Compared to control, the intervention group showed a significant mean decrease in (1) systolic blood pressure (SBP)—16.2 mm Hg (P ≤ .001), (2) respiratory rate—3.4 rpm (P < .001), and (3) heart rate—6.7 bpm (P ≤ .01). Heart rate variability parameters were improved in the intervention group, including high-frequency power (P = .01), the number of pairs of successive NN intervals that differ by more than 50 ms (ie, NN50, P = .01), and the proportion of NN50 divided by total number of NNs (ie, pNN50, P = .05).
Conclusions: Sheetali and Sheetkari pranayamas appear effective for lowering SBP in individuals with HTN. Within-group results suggest that the changes may be mediated through a modification in tone of the sympathovagal nervous system.
Prashanth Shetty, BNYS, MSc, PhD , is the principal of the Department of Clinical Naturopathy Diagnosis and Yoga Therapy and Research Methodology and Resent Advances, Sri Dharmasthala Manjunatheshwara College of Naturopathy & Yogic Sciences, in Belthangady, India. Kiran Kumar Reddy B, BNYS, MD, is an assistant professor in the Department of Modern Diagnosis and Obstetrics and Gynecology, Sri Dharmasthala Manjunatheshwara College of Naturopathy & Yogic Sciences. Lakshmeesha DR, BNYS, MD , is an assistant professor and the head of the research department at Sri Dharmasthala Manjunatheshwara College of Naturopathy & Yogic Sciences. Shiva Prasad Shetty, BNYS, MSc, is a professor in the Department of Yoga and Mind Body Medicine, Sri Dharmasthala Manjunatheshwara College of Naturopathy & Yogic Sciences. Selva Kumar G, BNYS, is an assistant professor in the Department of Principles of Yoga & Philosophy of Naturopathy, Sri Dharmasthala Manjunatheshwara College of Naturopathy & Yogic Sciences. Ryan Bradley, ND, MPH, is an associate professor and assistant director of research at the National University of Natural Medicine in Portland, Oregon, and he is an assistant professor in the Division of Preventive Medicine, University of California, San Diego, in La Jolla, California.
Corresponding authors: Prashanth Shetty, BNYS, MSc, PhD
E-mail address: sdmcnys@gmail.com
Ryan Bradley, ND, MPH
E-mail address: rbradley@nunm.edu
Hypertension (HTN) is a chronic medical condition in which the systemic arterial blood pressure (BP) is elevated, with stage I HTN defined as a systolic blood pressure (SBP) or diastolic blood pressure (DBP) greater than 140 mm Hg or 90 mm Hg, respectively.1 HTN is a major risk factor for stroke, myocardial infarction, heart failure, and arterial aneurysm and is a leading cause of chronic kidney failure.
Better BP control could lead to the prevention of 300 000 of the 1.5 million annual deaths from cardiovascular diseases in India.2 Essential HTN is the most prevalent form of HTN. Nearly 1 billion people, or approximately 26% of the adult population, have HTN worldwide, and HTN is common in both developed and undeveloped countries, affecting 333 million and 639 million individuals, respectively.3
The risk of HTN increases with age and, among individuals aged 60 years, its prevalence is approximately 65.4%.4 BP and adverse cardiovascular outcomes have been shown to be linearly associated, and a small reduction of 5 mm Hg in SBP corresponds to an approximately 25% reduction in cardiovascular events, including stroke and myocardial infarction.1
Although numerous drug and behavioral therapies are available to treat HTN, many of them are limited by cost, patients’ nonadherence, and/or side effects. The first line of treatment for HTN is preventive lifestyle changes, such as a low-sodium diet, physical exercise, and weight loss, which all have been shown to reduce BP significantly in people with HTN. 5
When HTN requires the immediate use of medications, lifestyle changes are recommended in conjunction with medication.4 Because large segments of the hypertensive population are either untreated or inadequately treated, nonpharmacological, alternative therapies with potential BP-lowering effects, such as yoga, deserve research attention.
India has a rich tradition of yogic practices. Comprehensive reviews have reported that yoga is potentially beneficial for patients with HTN. 6 It has the potential to reduce of BP through a combination of stress reduction and modification of the physiology of the autonomic nervous system. Pranayama is the art of prolongation and control of breath and helps bring conscious awareness to breathing patterns and the reshaping of breathing habits.7 Although yoga is typically thought of as a series of physical postures, a complete definition of yoga also includes breathing (pranayama), and meditation practices plus personal and societal behaviors.
Different types of pranayama can produce different physiological and cardiovascular responses in normal young individuals.8 Madanmohan et al9 and Pal et al10 have reported that training in slow, deep breathing has shown beneficial effects in lowering BP, after 3 weeks and 3 months, respectively. Studies have also reported beneficial effects for slow, deep breathing in reducing premature ventricular complexes in lowering BP.11 The findings of Madanmohan et al and Pal et al suggest that Chandranadi pranayamas are beneficial in reducing SBP plus are effective in reducing heart rate (HR) and respiratory rate in patients with HTN.12
Slowing the rate of breathing has been shown to be effectual in lowering BP in people with mild HTN, where it can be as effective as the use of medication.13 Clinical observations suggest that the Chandranadi pranayama practices of Sheetali and Sheetkari, or “cooling breath,” can reduce BP, and they do not result in any adverse effects.14 Notable differences exist between Chandranadi and Sheetali and Sheetkari pranayamas, which therefore deserves study. Chandranadi are practiced by breathing only through the left nostril, whereas Sheetali pranayama is practiced by inhaling cool air through a folded tongue and Sheetkari pranayama is practiced by inhaling air through the sides of the mouth through closed teeth.
Strong evidence also exists that a large proportion of patients with HTN have abnormalities in the function of the autonomic nervous system, typically increased sympathetic activity relative to parasympathetic tone. 15 This finding has been demonstrated with consecutive sympathetic and parasympathetic blockades of the heart16 and by spectral analysis of heart rate variability (HRV). 17 Therefore, measurement of HRV may provide valuable insights into potential mechanisms of pranayama practices on the regulation of BP.
Therefore, the present study aimed to measure the effects of Sheetali and Sheetkari pranayamas on BP, the autonomic nervous system, and respiratory functions among hypertensive participants.
Methods
Participants
Sixty individuals with HTN were recruited from the general population located in and around Ujire, Belthangady, Karnataka, India. The study was carried out at a clinical research center at Sri Dharmasthala Manjunatheshwara Yoga and Nature Cure Hospital (Belthangady, India).
To participate, candidates had to meet the following inclusion criteria: (1) aged between 25 and 65 years, (2) diagnosed with pre-HTN or stage I HTN—BP > 120/80 mm Hg, (3) being treated with medication, and (4) willing to provide informed consent.
Candidates were excluded from participation if they had: (1) secondary HTN; (2) a history, symptoms of, and/or laboratory reports suggestive of renal, neurologic, or ophthalmologic complications; (3) a history of known cardiac disease, including coronary artery disease, or participation in cardiac rehabilitation following bypass surgery; (4) prior exposure to pranayama practice; (5) a history of smoking or alcoholism; and (6) difficulty in rolling the tongue for Sheetali practice.
Eligible candidates signed an informed consent form prepared in English and Kannada. All procedures were approved by the Institutional Ethics Committee and were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
Procedures
The study was a randomized controlled clinical trial with pre- and postintervention evaluations following the 30-day study. The principal investigator screened and identified the 60 eligible participants. Enrolled participants were randomly allocated either to the intervention group or the wait-list control group. Randomization was accomplished by assigning each participant to a nonidentifying study identification (ID), randomly ordering the IDs, and then using a serial number generator to assign odd or even to each study ID. The odd-numbered participants were assigned to the intervention group, group 1—pranayama, and the even-numbered participants were assigned to the control group, group 2—quiet sitting.
Both groups completed baseline assessments. All participants were asked to follow a consistent diet for 30 days.
Group assignments were not concealed from the participants because the intervention was not possible to blind; however, group assignments were not known to the study’s coordinators or technicians collecting or analyzing the data.
Intervention
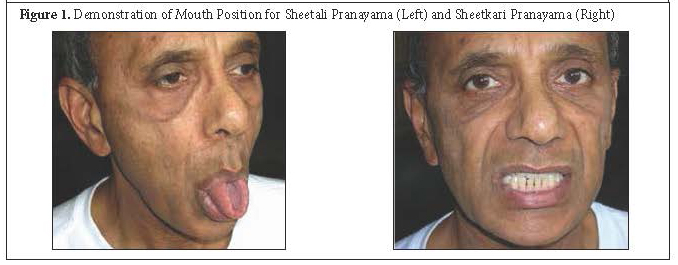
Participants who were randomly assigned to the intervention group were taught Sheetali and Sheetkari pranayamas. Each pranayama was demonstrated and practiced for 10 minutes each day, and the participants were observed by members of the research team. Those participants randomly assigned to the wait-list control group were asked to sit quietly for 20 minutes daily. An attendance record was maintained by monitoring the participation in the study by each participant on a daily basis. Table 1 describes the pranayama breathing instructions delivered in this protocol. Figure 1 demonstrates the mouth positions for the Sheetali pranayama and the Sheetkari pranayama.
Table 1. Pranayama Instructions and Procedure14
|
Sheetali Pranayama |
Sheetkari Pranayama |
|
Sit in a comfortable posture and close your eyes. Keep your hands on your knees throughout the practice. Protrude your tongue from your mouth and extend it to a comfortable distance. Roll its sides up so that it forms a tube. Breathe slowly and deeply through the tube-like tongue. Close your mouth at the end of inhalation and slowly exhale through your nose. Repeat the same process for 10 minutes daily. Follow the Sheetali practice with Sheetkari practice for 10 minutes daily. |
Sit in a comfortable meditative posture and close your eyes. Keep your hands on your knees throughout the practice. Press your lower teeth and upper teeth together and separate your lips as much as is comfortable. Breathe in slowly through the gaps in your teeth. Listen to the sound of your breath as the air is being drawn in. Close your mouth at the end of inhalation and slowly exhale through your nose. Repeat the process for 10 minutes daily. Repeat the sequence for 30 days. |
Outcome Measures
The following clinical assessments were performed per protocol at baseline and postintervention. Before the assessment, the participants were asked to sit and relax in a dimly lit, sound-attenuated cabin with a room temperature of approximately 30°C.
Blood Pressure. BP was recorded using a single mercury sphygmomanometer, auscultating over the right brachial artery, by a single research technician. All participants were required to sit still for 2 minutes with their feet flat on the floor and their backs supported during measurement.
Heart Rate Variability. An electrocardiogram (ECG) was recorded for 300 seconds using a 4-channel polygraph (Biopac, Bozeman, MO, USA; model No: BSL 4.0 MP 36). The Ag/AgCl pregelled electrodes (Medico Electrodes International, Noida, New Delhi, India) were placed as per the Limb Lead II configuration for recording the ECG. Data were acquired at the sampling rate of 1024 Hz and were analyzed offline. Noise-free data were included for analysis. HRV parameters that were collected and analyzed included both time and frequency domain analysis according to standard methods, specifically as follows:
· HR: Number of R waves per minute.
· R-R intervals: The distance between successive R waves measure in ms.
· SD R-R: The standard deviation of the R-R intervals.
· NN50: The number of pairs of successive R-Rs that differ by more than 50 ms.
· PNN50: pNN50, the proportion of NN50 divided by total number of NNs.
· High frequency: Most correlated with parasympathetic nervous system activity/tone.
· Low frequency: Correlated with both sympathetic and parasympathetic activity/tone.
· LF:HF: Ratio of low frequency to high frequency, providing an overall quantification of sympathetic tone.
Respiration Rate. Respiration was recorded using a volumetric pressure transducer fixed around the participant’s trunk at the level of the lower costal margin as he or she sat erect. Care was taken to adjust the strap such that the participant’s full inhalation was not restricted. Breath rate was calculated in cycles per minute by continuously counting the breath cycles during the 60-second epochs.
Data Analysis
Statistical analysis was done using SPSS software, version 21 (IBM Corp, Armonk, NY, USA). Data were checked for normal distribution and analyzed using the Shapiro-Wilk test for paired sample t test. Between-groups comparisons consisted of independent, 2-sided t tests of the mean pre- and postintervention change for each parameter of interest. Due the general weakness of the within-group comparisons, a conservative threshold of P ≤ .01 was considered significant for within-group changes in parameters of interest.
Results
Sixty hypertensive individuals, aged from 25 to 65 years, participated in the study, 30 in each group (Figure 2). No participants were lost to follow-up in this trial, and all participants completed at least 80% of all the study’s visits, based on attendance records from each practice session. Autonomic and respiratory variables were normally distributed and with equal variance. Table 2 shows within- and between-group comparisons for all a priori specified outcomes.
Table 2. Change in Heart Rate, Blood Pressure, and Heart Rate Variability
|
Variables |
Intervention Group (n = 30) |
Wait-list Control Group (n = 30) |
|||||
|
Preintervention Mean ± SD |
Postintervention Mean ± SD |
P Value a |
Preintervention Mean ± SD |
Postintervention Mean ± SD |
P Value a |
P Value b |
|
|
HR |
74.0 ± 6.6 |
67.3 ± 7.8 |
.01 |
70.5 ± 15.9 |
71.2 ± 16.0 |
.57 |
.009 |
|
Respiratory rate |
14.9 ± 1.0 |
11.5 ± 1.0 |
.001 |
16.1 ± 1.4 |
15.8 ± 2.2 |
.55 |
.005 |
|
SBP |
148.2 ± 7.9 |
132.00 ± 3.8 |
.001 |
153.6 ± 9.5 |
152.9 ± 9.8 |
.08 |
.0009 |
|
NN50 |
97.6 ± 173.3 |
107.30 ± 55.3 |
.01 |
87.2 ± 146.3 |
66.7 ± 37.8 |
.68 |
.54 |
|
pNN50 |
22.1 ± 38.8 |
9.6 ± 13.3 |
.05 |
3.9 ± 8.9 |
5.9 ± 1.5 |
.68 |
.07 |
|
HF |
40.2 ± 27.4 |
75.0 ± 17.5 |
.01 |
39.5 ± 18.0 |
26.8 ± 17.4 |
.81 |
.38 |
|
LF:HF ratio |
3.3 ± 3.7 |
2.4 ± 1.5 |
.05 |
3.1 ± 4.8 |
5.0 ± 4.6 |
.65 |
.50 |
a P values are for 2-sided t tests of differences within groups.
b P values are for 2-sided t tests of change in each parameter (pre-post) between groups.
Abbreviations: HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; RMSSD, root mean square of successive differences; RR, R-R interval; NN50, the number of pairs of successive NN intervals that differ by more than 50 ms; pNN50, the proportion of NN50 divided by total number of NNs; LF, low frequency; HF, high frequency
Significant differences existed between groups in HR (P = .009), respiratory rate (P = .005), and SBP (P = .0009). For the intervention group, DBP was also reduced; however, the difference between groups was not statistically significant. The evaluation of the HRV parameters demonstrated multiple changes in the intervention group, including (1) increases in the proportion of the number of pairs of successive NN intervals that differed by more than 50 ms, divided by total number of beat-to-beat (NN)s PNN50, with P ≤ .05; (2) a reduced low-frequency/high-frequency ratio (LF/HF), with P ≤ .05; (3) increases in the number of pairs of successive NNs that differed by more than 50 ms (NN50), with P ≤ .01; and (4) increases in HF, with P ≤ .01. Differences between groups in the HRV parameters were not statistically significant, although the HRV parameters in the intervention group did change in a favorable direction compared with the control group (eg, increased NN50 and decreased pNN50).
Discussion
The current research demonstrates a significant decrease in HR, RR, and SBP, which suggests improved psychophysiological relaxation following the combination of 2 pranayama techniques. The results may be due to a normalization of the autonomic cardiovascular rhythms, with increased vagal modulation and/or decreased sympathetic activity, together with improvement in baroreflex sensitivity. However, that hypothesis is based on preliminary findings in the intervention group and requires confirmation.12
The results of Madanmohan et al21 demonstrated that yoga practice with pranayama has numerous beneficial effects on the body but especially on balance between the sympathetic and parasympathetic nervous systems (ie, it gives a calming effect by reducing stress). According to Hanson et al,22 pranayama increases both alpha and beta brainwave activity at the beginning of the practice, suggesting increased awareness and increased relaxation at the time. Chandranadi pranayama appears effective in reducing HR and SBP in hypertensive patients on regular standard medical management, and similar changes in HR and SBP to those observed from Chandranadi practice were also observed in the current study. 12
Swami Swatmarama claimed that Sheetali and Sheetkari pranayamas bring about a cooling effect mediated through increased parasympathetic activity, with decreased RR and BP being attributed to the predominant vagal tone following slow-breathing techniques.14 The increase in HF in the current intervention group suggests an increase in parasympathetic activity, and the increased NN50 suggests that the Sheetali and Sheetkari pranayamas improved the cardiac tone of hypertensive patients; however, these observations deserve confirmation in larger, definitive trials.
The current trial was strengthened by its randomized design, the close monitoring of practice adherence, and the moderate length of the intervention. However, given the variability in HRV parameters, the trial remained limited by its modest sample size, which may have impacted the current research team’s ability to measure additional, significant between-group differences. Another limitation was that data were not collected during the practices to assess SBP or HRV parameters and, therefore, the research team was able only to measure any effects that persisted beyond the practice itself.
Future research is in the design stages to confirm the promising results measured in the current preliminary clinical trial. Replicative research in additional populations is particularly needed to determine if the measured results are generalizable and if the intervention is tolerable in adults less culturally attuned to yogic practices than adults in India.
The current results demonstrated that Sheetali and Sheetkari pranayama may be beneficial for hypertensive participants, by reducing BP and R-R interval and also shifting autonomic balance in favor of parasympathetic dominance. To the best of the current research team’s knowledge, no previous reports on the effects of Sheetali and Sheetkari pranayamas in patients with HTN have been published. Additional clinical research is required to replicate the current findings and establish a deeper understanding of the mechanisms involved. Future research will determine if this simple and low-cost technique can reduce BP in generalizable samples of people with HTN. If so, Sheetali and Sheetkari pranayamas may be a useful self-care practice to recommend for people with HTN.
Conclusion
Sheetali and Sheetkari pranayamas reduced SBP in adults of southern Indian descent with HTN. Sheetali and Sheetkari may also alter parameters of HRV, with preliminary results suggesting improved parasympathetic-to-sympathetic balance. Larger samples are required to confirm or refute the measured results in HRV parameters. Given the low risk and apparent clinically meaningful effects of a >5 mm Hg reduction in SBP, additional clinical research on pranayama, an established limb of yoga, is warranted.
Acknowledgements
The current research team thanks their parents for their unconditional love and support. They are thankful to Padmavibhushana Poojya Dr D. Veerendra Heggadeji, president of the Sri Dharmasthala Manjunatheshwara Educational Society in Ujire, India, for their blessings. They thank all the participants for their cooperation.
References
1. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
2. Zeng C, Villar VA, Yu P, Zhou L, Jose PA. Reactive oxygen species and dopamine receptor function in essential hypertension. Clin Experimen Hypertens. 2009;31(2):156-178.
3. Longo D, Fauci A, Kasper D, Hauser S, Jameson J. Harrison’s Principles of Internal Medicine. 19th ed. New York, NY: McGraw-Hill; 2011.
4. Whelton PK, He J, Appel LJ, Cutler JA, et al. Primary prevention of hypertension: Clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288:1882-1888.
5. Luma GB, Spiotta RT. Hypertension in children and adolescents. Am Fam Physician. 2006;73(9):1558-1568.
6. Innes KE, Baurguinon C, Taylor AG. Risk indices associated with the Insulin resistance syndrome, cardiovascular disease and possible protection with yoga: A systematic review. J Am Board Fam Pract. 2005;18(6):491-519.
7. Bjlani RL. Understanding Medical Physiology. New Delhi, India: Jaypee Brothers; 2004.
8. Shannahoff-Khalsa DS, Kennedy B. The effects of unilateral forced nostril breathing on the heart. Int J Neurosci. 1993;73:47-60.
9. Madanmohan, Udupa K, Bhavanani AB, Vijayalakshmi P, Surendiran A. Effect of slow and fast pranayamas on reaction time and cardio respiratory variables. Indian J Physiol Pharmacol. 2005;49(3):313-318.
10. Pal GK, Velkumari S. Madanmohan, effect of short term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120(2):115-121.
11. Prakash ES, Ravindra PN, Madanmohan, Anilkumar R, Balachander J. Effect of deep breathing at six breaths per minute on the frequency of premature ventricular complexes. Int J Cardiol. 2006;111(3):450-452.
12. Ananda BB, Zeena S. Immediate effect of Chandranadi pranayama (left unilateral forced nostril breathing) on cardiovascular parameters in hypertensive patients. Int J Yoga. 2012;5(2):108-111.
13. Sydorchuk L, Tryniak M. Effect of voluntary regulation of the respiration on the functional state of the autonomic nervous system. Lik Sprava. 2005;1(2):65-68.
14. Swami M. Hata Yoga Pradipika. Bihar, India: Bihar School of Yoga, Yoga Publications Trust; 2013.
15. Julius S, Majahalme S. The changing face of sympathetic overactivity in hypertension. Ann Med. 2000;32:365-370.
16. Julius S, Pascual AV, London R. Role of sympathetic inhibition in the hyperkinetic type of borderline hypertension. Circulation. 1971;44:413-418.
17. Pramanik T, Sharma HO, Mishra S, Mishra A, Prajapati R, and Singh S. Immediate effect of slow pace Bhastrika pranayama on blood pressure and heart rate. J Altern Compliment Med. 2009;15(3):293-295.
18. Madanmohan. Effect of yogic practices on different system of human body. Ind J Physiol Pharmacol. 2008;52:164-170.
19. Hanson R. Pranayama brain studies. Love to Know Web site. http:// yoga.lovetoknow.com/Pranayama_Brain_Studies. Accessed September 6, 2017.
All rights reserved. Terms and Conditions.