Successful Interprofessional Treatment of Juvenile Rheumatoid Arthritis: A Case Report
Judith Boothby, MS, DC, PC; Shelly Coffman, PT, DPT, OCS, FAAOMPT, CSCS; Todd Turnbull, DC
Abstract
A 9-y-old boy with severe juvenile rheumatoid arthritis who had been recommended for bilateral hip replacement received treatment for more than 8 y from an interprofessional group of clinicians. The clinicians provided chiropractic, naturopathic, and acupuncture care, in addition to pediatrics, rheumatology, orthopedics, and physical therapy care. This process was not easy; the patient used crutches for 2 y during treatment and experienced severe pain secondary to multiple joint pathology. He is now aged 17 y, and he regularly plays golf and basketball with his own hips.
Judith Boothby, MS, DC, PC, is a chiropractor at Third Way Chiropractic in Portland, Oregon; Shelly Coffman, PT, DPT, OCS, FAAOMPT, CSCS, is is a physical therapist at 360° sports medicine and spine therapy in Portland Oregon; Todd Turnbull, DC, is is a chiropractor at the Turnbull Clinic in Portland Oregon.
Corresponding author: Judith Boothby, MS, DC, PC
E-mail address: boothbyj@yahoo.com
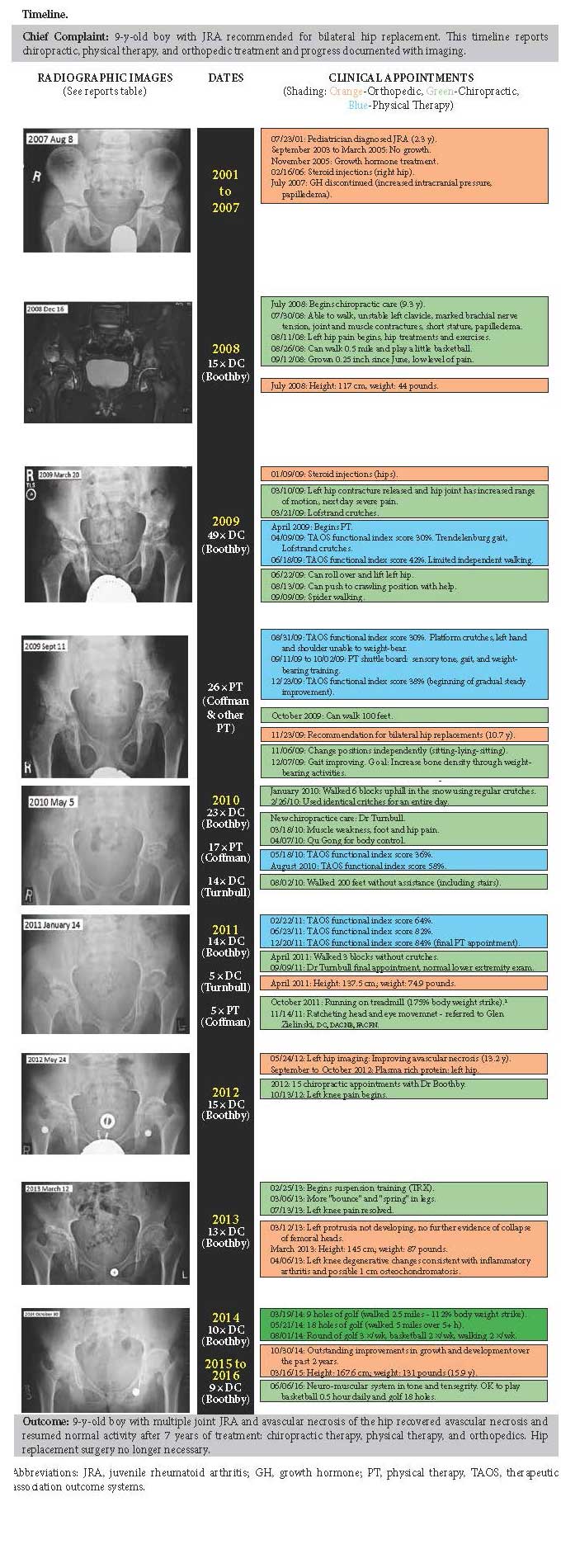
Patient Care Narrative
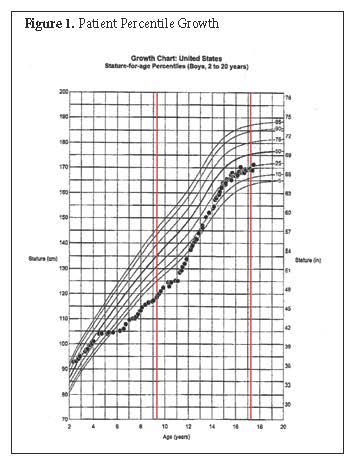
This 9-year-old boy initially showed signs of systemic juvenile rheumatoid arthritis (JRA) at 2 years of age. His rheumatoid factor was negative at that time. Since first diagnosed in 2001, he had multiple diagnostic procedures including lumbar puncture and received multiple treatments including medications and joint injections. He was given growth hormone when his growth stopped (Figure 1) and subsequently developed papilledema and a rise in intracranial pressure. Radiographic imaging (see Timeline) revealed bilateral hip and right shoulder involvement of JRA along with blocked spinous process of his cervical spine. The orthopedic surgeon was concerned but willing to follow changes in the patient rather than recommend surgical interventions.
In 2008, when Judith Boothby, DC, initiated treatments, the patient needed assistance changing positions during treatments. Biomechanically, his upper body was not supporting his trunk, which altered load-bearing. His hip movement was restricted, and his right quadriceps was atrophied. Initial treatment goals were to restore his breathing capacity and increase an awareness of, and connection with, his body. The treatments included specific tissue mobilizations to create differentiation between his muscles, nerves, joint capsules, and ribs. The patient also performed specific exercises at home. After 2 months of treatment, laboratory testing for inflammatory biomarkers (C-reactive protein, erythrocyte sedimentation rate) were normal without steroids. After 7 months of treatment, he rotated his hips for the first time, although this movement was accompanied by intense pain. He was referred to physical therapy for additional support.
In April 2009, the patient began treatment with a physical therapist—Shelly Coffman, DPT, at PT-360—to develop basic movements related to activities of daily living. The patient was using Lofstrand crutches to assist with weight bearing and had a Trendelenburg gait, and his left foot “toed-in” when physical therapy was initiated. He experienced significant pain in his left hip, which was internally rotated and flexed with limited range of motion. In addition, he had limited shoulder mobility and needed moderate assistance with transfers. On physical examination, left hip muscle testing revealed decreased strength (3/5), which was painful. Moderate restriction was noted to the left anterior and inferior hip capsule. Therapeutic Associates Outcomes System (TOAS) functional score at the time he began physical therapy was 30%, with pain 7/10 on a visual analog scale. The patient also demonstrated a positive Ober and Thomas test with his left hip. Strengthening of the gluteal muscles and trunk to shift mechanical strain away from the inflamed hip joints was the primary treatment goal.
Ober test is utilized to assess for tightness of the lateral hip and thigh musculature using side lying bent knee leg adduction.
Thomas test is for psoas hypertonicity or hip contracture. The patient lies on their back with the one side hip and knee flexed while lowering the other leg to the table. The test is positive when the leg does not get to to full neutral or extension and the sacrum and ilium are not maintained in contact with the table.
For 1 month in August 2009, this patient was referred to New Heights Physical Therapy Plus to use the “Shuttle Balance System,” which worked to improve the engagement of his legs. The Shuttle Balance System is a safe unstable platform that is used in vestibular, balance, vision, and proprioceptive training programs. The movement of the platform simulates a slip through motion in all horizontal planes in standing and seated positions.
The patient was seen in physical therapy with Dr Coffman weekly for the first 4 months, every other week, for months 5 to 11, and then once per month for 1 year. Physical therapy treatment was expanded to include rheumatoid arthritis joint management of his hips, shoulders, and cervical spine.
Shortly after this patient turned 10 years old, a new orthopedic specialist recommended bilateral hip replacement secondary to concern regarding the risk of acetabular fracture. The patient and his parents chose to continue with chiropractic care, physical therapy, and other nonsurgical medical interventions. Initial TAOS functional score was 30% (postintervention 2.5 years later, the TAOS score was 84%).
In March 2010, concurrent with physical therapy this patient was referred to Todd Turnbull, DC, CCSP, for strengthening the use of his body. The patient presented using crutches with difficulty balancing, walking, and standing. Physical examination used eccentric break testing protocols for bilateral muscle testing. Test results measurement guidelines were as follows: 5 = full isometric lock and hold, 4 = notable isometric lock, 3 = breaks with strong resistance, 2 = breaks with moderate resistance, and 1 = breaks with minimal resistance. Initial testing revealed grade 1 dysfunction of the left iliacus, left psoas, gluteus medius bilaterally, abductors bilaterally, and right sartorius. Grade 2 muscle power output was noted in the quadriceps and adductors bilaterally. Chiropractic neuromuscular integration manipulations were performed—this is nerve proprioceptors stimulation to eliminate the autogenic inhibition reflex, reduce muscle tension, and restore muscle power output. Overall, interventions were designed to support and encourage global function by addressing the hip joints and supporting musculature, the lower extremities, and other areas of the body as needed. The patient was seen 1 to 2 times per month for 9 months and at the same time learned qigong exercises as a self-management tool using breathing to consciously connect his mind and body. In the course of treatments, the patient’s hip and pelvic muscles increased power output and maintained pain-free ranges of motion except after performing a moderate amount of activity. Left psoas strength testing noted improvement from grade 1 to a grade 4. Gait improved to walking without crutches and playing a minimal amount of basketball. Symptoms of hip and leg pains were reported only after moderate exertion.
Once during a snow storm, his parents had to park at the bottom of the hill that they lived on and walk up the hill. This 6-block walk was a triumph and encouraged him; subsequently, he began to feel better and his diet improved. By the end of 2011, his TAOS score was 84% and he had completed his physical therapy with Dr. Coffman and his and chiropractic treatments with Dr Turnbull.
Often in his course of recovery improvement in one symptom may be followed with a new symptom. In this case, the patient developed ratcheting head movement. His head would turn with jerky movements. This symptom can be from functional neurological imbalances causing uneven motor regulation to the upper neck muscles. He was referred to Glen Zielinski, DC, DACNB, FACFN, for a functional neurology evaluation and treatment, which resolved the ratcheting head movement. Radiologic imaging in May 2012 showed improvement of the avascular necrosis in his hips. Then, as his left hip improved and activity increased, he developed left knee pain. Magnetic resonance imaging suggested rheumatic flare-up, partial avulsion of anterior cruciate ligament, and osteochondromatosis. His chiropractic treatment with Dr. Boothby was designed to restore internal rotation of his tibia and in 9 month, his left knee pain resolved. In May 2014, this patient was now 15 years old and playing 18 holes of golf on the varsity golf team and could play basketball—all with his own hips. He continued treatments with Dr Boothby for an addition
2 years while he continued to grow.
Discussion
Certain medications, such as methotrexate and tumor necrosis factor inhibitors, have helped to achieve disease remission earlier in the disease course of JRA and have reduced hospitals stays by 50%, thus reducing the population of young people needing total hip replacement.3 Even with these medication improvements, approximately 10% of juvenile idiopathic arthritis patients have end-stage degeneration changes that require total hip arthroplasties.1 The risks to arthroplasty in addition to the surgery include infection, dislocation, deep vein thrombosis, epidural anesthesia, and bone grafting. Owing to the small size of his bone, there could be loosening of the implant and the need for future surgeries. After surgery, there would not be further growth in the hips because the growth plates will be closed. Rheumatoid arthritis continues to pose a substantial humanistic and economic burden on patients, and there are still unmet needs.4
Multiple degenerated hip shoulder joints and blocked spinous processes on X-ray show only the tip of the iceberg. The deeper story is an inflammatory process happened at such an extent that his body formed adhesions between the many fascial layers in his neck, hands, feet, hips, and shoulders. His basic body mechanics were altered enough that he had not developed adequate body stability and control. With an active rheumatoid arthritis process in this patient whose joints were continuing to develop and grow, with significant weakness against gravity, poor coordination and function in gait and activities of daily living, significant training and guidance was required to shift mechanical stresses away from involved and painful joints by improving strength and motor recruitment, addressing gait imbalances. and patterning and enabling greater use of mechanical coupling patterns to gain function and strength.
The normal, healthy growth of this patient’s bone, joint, muscle, and nervous structure was supported and encouraged by integrating multiple therapies providing the opportunity to reduce the inflammatory process and increase the load bearing capacity, thereby allowing the body to heal itself. The different perspectives of the practitioners supported this patient as his healing needs changed. The chiropractic treatment goals were to systematically relive adhesions between fascial planes and to mobilize joints. This would allow the body to build stability in a compressive load and to restore joint movement and muscular control of that movement. This was not a linear process and required therapeutic adaptation.
For example, when his left hip moved, he had very little ability to balance the movement of his hip. The adjustment of his left hip was not painful, but the aftermath of restoring hip movement was excruciating for him. That was not foreseen. Then his left knee had a rheumatoid arthritis flare and he had X-ray evidence of a calcific cruciate ligament. Then he had ratcheting head movement. The treatment was really about his hips but, to help his hips, we had to treat his whole body. Any one of these problems on this treatment path could have been a significant lifetime lesson for someone else. Yet each step was a significant part of the healing of his hip. His hips could not work correctly until his knee and head moved correctly.
Conclusion
Training and guidance were required to shift the mechanical stresses in this patient with JRA whose joints were continuing to develop and grow in the presence of significant weakness, poor coordination and function in gait, and activities of daily living. Research into interprofessional collaborative care for JRA patients is needed. It would be useful to minimize joint degeneration through the incorporation of biomechanical knowledge and functional neurology along with strategies for the treatment of fragile patients.
Acknowledgements
This case report was written without grant support by Judith Boothby with support from Melissa Barber and David Riley.
References
1. Abdel MP, Figgie MP. Surgical management of the juvenile idiopathic arthritis patient with multiple joint involvement. Orthop Clin North Am. 2014;45(4):435-442.
2. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley DS, CARE Group. The CARE guidelines: Consensus-based clinical case report guideline development. Global Adv Health Med. 2013;2(5):38-43.
3. Len Harty, Gary O’Toole, Oliver FitzGerald. Profound reduction in hospital admissions and musculoskeletal surgical procedures for rheumatoid arthritis with concurrent changes in clinical practice (1995-2010). Rheumatology. 2015;54:666-671.
4. Taylor PC, Moore A, Vasilescu R, Alvir J, Tarallo M. A structured literature review of the burden of illness and unmet needs in patients with rheumatoid arthritis: a current perspective. Rheumatol Int. Rheumatol Int. 2016;36(5):685-695.
All rights reserved. Terms and Conditions.

